Praxis, also known as motor planning, is the ability to combine information from the environment and successfully perform actions to completion. Despite this brief definition, the ability to perform praxis is quite involved. Occupational therapists often break praxis abilities down into specific parts.
Praxis – Ideation
Part one is called ideation, in which we use varying brain functions to support ideas. Ideation is the ability to grasp what is being seen and develop an idea as how to use objects in the environment to develop a course of action. How to spot ideation? Look at how your child plays with simple items. Is there intention and a bit of complexity to the moves? Can the blanket switch hands, fold up, cover different body parts, become a tent, etc.? If struggles are apparent with several items, and play appears limited, it may be due to ideation.
Arousal and Rhythmicity
Part two is arousal and rhythmicity. We need to be able to perform actions in a rhythmical manner. We also need to match our arousal or energy to the rhythm to perform. Difficulty with rhythmicity is often most apparent in how a child times their movement. People may describe children who struggle in this area as clumsy.
Complete Movement Efficiently
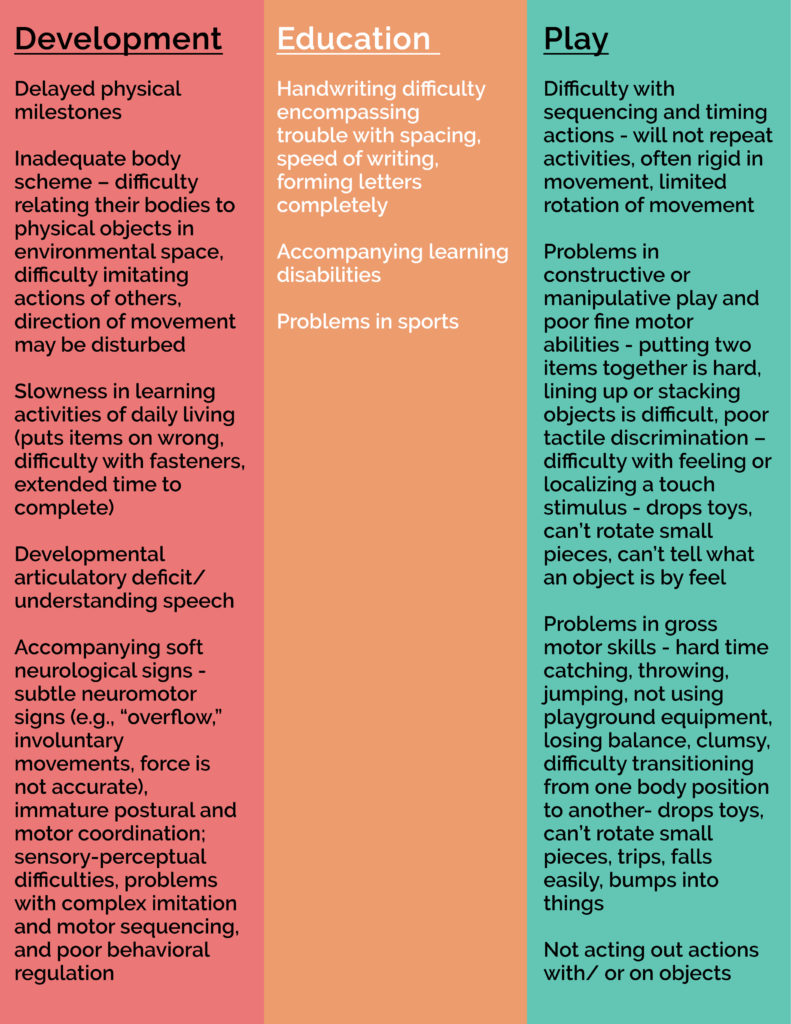
Part three is the ability to complete or execute the movement efficiently. Planning and sequencing movements with the ability to make real-time adaptions is the foundation for learning a multitude of skills. To help get a better idea of what a motor difficulty may look like, see the chart below.
When a difficulty is present in any one of these parts, it will affect the overall presentation of movement. Professionals use a variety of terms to describe the difficulties observed, including dyspraxia, developmental dyspraxia, coordination, or perceptual motor difficulties. Some children will end up with a diagnosis of Developmental Coordination Disorder. Meanwhile, others who present with difficulties will not have a diagnosis.
Regardless of the confusing terms, OTs are one group of therapists with the skills to address such motor issues in children. Therefore, they have specialized skills in understanding primitive reflexes, motor control based on neurological components, sensory processing, and perceptual processing. Our occupational therapists will assess which parts are leading to the difficulty and then help remediate the difficulty with fun and engaging activities. Above all, remember that it is never too late to address motor challenges! The positive outcomes can be considerable for a child. Lastly, if you have concerns, reach out to MOSAIC today to schedule a free screen or a full evaluation.
References
dyspraxiausa.org
www.dyspraxiafoundation.org.uk
Dyspraxia from an Occupational Therapy perspective by Natasha Patten BSc (Occupational Therapy)
CE-Article- September-2019.pdf (aota.org)

