Understanding Toileting Accidents and the Extremes
 Childhood bladder and bowel issues are more common than one would think. Understanding toileting accidents can help improve how you approach problems. I remember going through this experience with my own son and wondering what the heck was going on? He was 3 years old, and he would not poop. I knew he was scared. I knew he was getting stressed out. Also, I knew he was going up to 7 days without pooping!! I remember questioning if he needed more fiber, fluid, exercise. As time passed, I worried that there would never be a day when he did not need to take Miralax. I worried how much he was being mentally affected by all the stress around pooping. I think every family member weighed in at some time; all with good intentions but no real facts or practical help.
Childhood bladder and bowel issues are more common than one would think. Understanding toileting accidents can help improve how you approach problems. I remember going through this experience with my own son and wondering what the heck was going on? He was 3 years old, and he would not poop. I knew he was scared. I knew he was getting stressed out. Also, I knew he was going up to 7 days without pooping!! I remember questioning if he needed more fiber, fluid, exercise. As time passed, I worried that there would never be a day when he did not need to take Miralax. I worried how much he was being mentally affected by all the stress around pooping. I think every family member weighed in at some time; all with good intentions but no real facts or practical help.
I will spare you all the various ups and downs along our journey. I will skip ahead to inform you that we did survive that stage of his development relatively unscathed. But I regret that we (my husband and I) were not aware of this topic. I regret that we didn’t get help for our son sooner. The experience led me into learning more about this therapy area. Now I am helping families talk more openly about poop and pee issues!!
Understanding Childhood Bowel and Bladder Disorders and Accidents
Elimination disorders are disorders that are typically related to body part function. They are not necessarily due to a specific condition or disease. The most common disorders include:
- Urinary incontinence
- Urinary retention
- Constipation
- Constipation leading to encopresis (poop that is backed up into colon for longer periods of time)
- Fecal incontinence
- Bedwetting
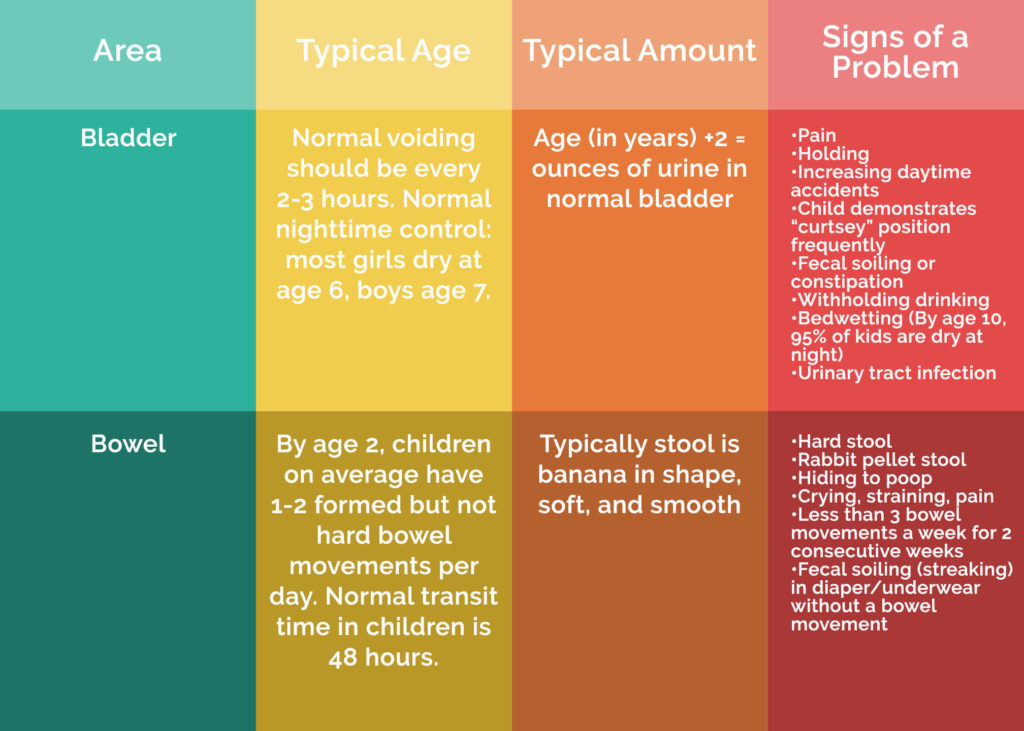
Many of these disorders appear around the time of toilet training and in preschool age. The symptoms vary by disorder and by child. The intensity and severity are also child/family specific. If the specific disorder is not addressed, the disorder and the subsequent behaviors and physical symptoms can occur indefinitely. It is important to know that most children do not “outgrow” the disorder. Therefore, they need help.
First off, it is necessary to seek medical advice (see symptom guide provided) and increase your understanding of what is happening for your child. As a parent, I wish the two following recommendations were addressed after our son was diagnosed with encopresis:
- Medical interventions that are needed.
- Rehabilitation treatment options are available and successful.
Understanding Treatment Options for Toileting Accidents
- Bowel/bladder retraining – habit training, pelvic floor muscle training or re-training, biofeedback, postural training, and breathing education/training
- Dietary/fluid education
- Feeding therapy
- Behavioral modification
- Understand that potty training needs to be reviewed. A plan needs to be established that fits the child’s needs
Had I known and understood these two areas before, I would have handled our experience differently. We would have had success earlier on. If you have concerns for your child, please view the symptoms guide. Then, use the resources provided to choose your best course of action.
How do we treat here at MOSAIC?
If we recognize a disorder, it is important to look at the age and development of the child we are treating and establish realistic***goals. Occupational and physical therapists specifically trained in this area can establish comprehensive treatment plans. Firstly, we are looking to increase your child’s and family’s success and independence in the area of toileting. Secondly, we will collaborate with you in addressing the daily routines and training needs for your family. Thirdly, we will assess your child’s environment. The therapist will provide you with the best positioning for sitting on the toilet. They will also provide support to improve your child’s daily experience. Finally we will address behaviors surrounding resistance and avoidance. We will also teach you how to support improved habits and patterns.
Collaboration with your child’s primary care provider will occur. This provides continuous care for diet and medication follow through. We may design specific physical pelvic floor muscle training exercises. Exercises will improve strength and “coordination” of the muscles needed to support elimination of urine or stool. We will develop a home program with you to support the individual goals for your child. In addition, we will include toilet training support and education in our treatment approach. However, you should be aware that toilet training is more about the parent than the child.
***Realistic goals are about measuring success through reduced symptom occurrence and physical improvements. Therefore, goals are NOT about being toilet trained by a specific date. Toilet training includes a child’s ability to respond to bodily urges in a timely manner. This often does not fully occur until later in development (ages 4-5).
Resources
In conclusion, for more help understanding toileting accidents, check out bedwettingandaccidents, GIKids, The Poo in You, and the Bristol Stool Scale. Or, call MOSAIC to set up an appointment with a physical or occupational therapist trained in this area.
References
-
An Introduction to Pediatric Bladder and Bowel Disorders, Part 2 Tiffany Ellsworth Lee, MA, OTR, BCB-PMD, PRPC
-
An Introduction to Pediatric Bladder and Bowel Disorders, Part 1 Tiffany Ellsworth Lee, MA, OTR, BCB-PMD, PRPC
-
Physical Therapy Management of Pediatric Incontinence Jennifer Stone, PT, DPT, OCS, PHC
