What is working memory and how does it relate to language? Working memory refers to the brain’s process of storing information, then recalling the information later on to complete tasks. It’s a storage system used for tasks of daily living, including engaging in conversation, following instructions, and solving problems. For example, if you ask your child “what’s 2+2?” Your child uses working memory to process the question, implement a previously learned skill to execute the calculation, then respond. Working memory is often confused with short term memory. Working memory involves the process of storing, organizing, and manipulating information for use later on. Short term memory involves temporary storage of information.
What is working memory and how does it relate to language? Working memory refers to the brain’s process of storing information, then recalling the information later on to complete tasks. It’s a storage system used for tasks of daily living, including engaging in conversation, following instructions, and solving problems. For example, if you ask your child “what’s 2+2?” Your child uses working memory to process the question, implement a previously learned skill to execute the calculation, then respond. Working memory is often confused with short term memory. Working memory involves the process of storing, organizing, and manipulating information for use later on. Short term memory involves temporary storage of information.
Working memory allows an individual to process language that is heard or seen. When a sound, word, or sentence is heard or seen, working memory holds this information in the brain. It then retrieves corresponding information from the long term memory and processes the new and old information together. If the information heard or seen is new, the working memory will store it to long term memory. Ideally, this new information can be used to make associations with information stored in the long term memory for use later on.
What is processing speed?
Processing speed is a basic cognitive skill. It refers to the amount of time that it takes for an individual to complete a mental task. Otherwise, it is defined as the speed by which an individual can understand and react to information that is heard or seen. If an individual’s processing speed is slow, they may experience greater difficulty processing information quickly and efficiently in order to think and learn.
Ways that we use working memory and processing speed:
We use working memory in a variety of ways to participate in activities of daily living. This includes, but is not limited to:
- Responding in conversation
- Following instructions
- Verbal comprehension
- Reading comprehension
- Reading a new word
- Paraphrasing information
- Organizing activities of daily living
- Problem solving (e.g. calculating a math problem in your head)
How does working memory and processing speed impact language?
Working memory and processing speed are crucial to language learning and use. Research disagrees on whether working memory and processing speed are the cause of language impairments. However, we do know that some (but not all) children with language impairments demonstrate poor working memory and processing speed. This tells us that we need to consider these skills when working with language impairments.
Working memory and processing speed are related to overall academic success. Working memory and processing speed correlate to comprehension and vocabulary. Specifically, vocabulary/word learning, working memory, and processing speed. Research reveals that children with good working memory and processing speed are better word learners.
Addressing working memory and processing speed related to language:
Research does not suggest that training working memory or processing speed will improve language. Instead, it suggests that we support working memory and processing speed using a strategy based approach. Firstly, we need to identify the working memory and processing speed demands of the environment and task. Then, we must provide supports to decrease demands for those children with language impairments. This might include: use of repetition, decreased instruction rate, task lists, detailed instructions, or use of visual supports. Use of supports will help provide children with strategies to manage their working memory and processing speed within the context of the environment or task. Meanwhile, intervention should remain focused on their language needs.
Strategies used to improve memory when addressing language:
Children are capable of learning memory techniques at a young age. Some positive techniques to use in therapy and at home include:
- Visualization – taking mental “pictures” of something heard or seen
- Rehearsal – repeating something aloud or to oneself over and over
- Chunking – remembering items, such as a phone number, in groups
- Visual reminders – use Post-It notes, calendars, schedules, or alarms
Memory games can also support a child’s ability to practice the strategies that they have learned in therapy. For additional information on working memory, processing speed, and language, seek support from your child’s therapist. The most appropriate supports, strategies, and memory games to use with your child will be determined by your therapist. Implement strategies and practice daily across a variety of activities and environments.
If you have concerns about your child’s working memory or processing speed, call MOSAIC to set up an evaluation with one of our speech-language pathologists.
References:
-
Abel, A. (2017). Guest post: Working memory, processing speed, and language disorder. The Informed SLP Blog. Retrieved online on 12/22/2020.
-
Boudreau and Costanza-Smith. (2011). Assessment and Treatment of Working Memory Deficits in School-Age Children. Lang Speech Hear Serv Sch.2011; 42: 152-166. Retrieved online on 12/22/2020.
-
Kid Sense Child Development Corporation Pty Ldt. (2020). Working Memory. Retrieved on 12/22/2020.
-
Speech Therapy Talk Services, LLC. (2020). Making Speech Therapy Meaningful. Working Memory. Retrieved online on 12/22/2020.

 Like any profession, you have to start somewhere. Starting out as a “new” anything is always challenging and so exhausting mentally. The transition from title of “student” to “new grad practitioner” poses many challenges related to the actual work, as well as adjusting to new changes in your personal schedule as well. Being a new graduate has had an interesting spin in 2020 with ever changing schedules and all the uncertainty surrounding COVID-19. Put that on top of a new grad, and you have a recipe for extra naps in your day. Here are some ideas, tips, and resources for new graduates that may help with the difficult transition. At the bottom of this blog, hear some bonus words of wisdom through interviews from fellow new grad pediatric and adult practitioners across Montana.
Like any profession, you have to start somewhere. Starting out as a “new” anything is always challenging and so exhausting mentally. The transition from title of “student” to “new grad practitioner” poses many challenges related to the actual work, as well as adjusting to new changes in your personal schedule as well. Being a new graduate has had an interesting spin in 2020 with ever changing schedules and all the uncertainty surrounding COVID-19. Put that on top of a new grad, and you have a recipe for extra naps in your day. Here are some ideas, tips, and resources for new graduates that may help with the difficult transition. At the bottom of this blog, hear some bonus words of wisdom through interviews from fellow new grad pediatric and adult practitioners across Montana. The first part in the postnatal return to running series after childbirth will address signs and symptoms of pelvic floor and/or abdominal wall dysfunction as well as risk factors. One question that frequently gets asked is, “When can I start running after giving birth?” Some women can’t fathom running soon after birth and some go in way too quickly! Running is a high impact sport that places a lot of demand on the body. High impact exercise was found to have a 4.59 fold increased risk of pelvic floor dysfunction compared to low impact exercise. After birth, women need adequate time to heal and regain strength, specifically with abdominal and pelvic floor muscles. This includes women who had vaginal births and caesarean section deliveries!
The first part in the postnatal return to running series after childbirth will address signs and symptoms of pelvic floor and/or abdominal wall dysfunction as well as risk factors. One question that frequently gets asked is, “When can I start running after giving birth?” Some women can’t fathom running soon after birth and some go in way too quickly! Running is a high impact sport that places a lot of demand on the body. High impact exercise was found to have a 4.59 fold increased risk of pelvic floor dysfunction compared to low impact exercise. After birth, women need adequate time to heal and regain strength, specifically with abdominal and pelvic floor muscles. This includes women who had vaginal births and caesarean section deliveries! Voice is one aspect of communication. The sound of our voice is also something with which we identify strongly. It is uniquely us. But like the rest of our body, our voice changes with normal aging.
Voice is one aspect of communication. The sound of our voice is also something with which we identify strongly. It is uniquely us. But like the rest of our body, our voice changes with normal aging.

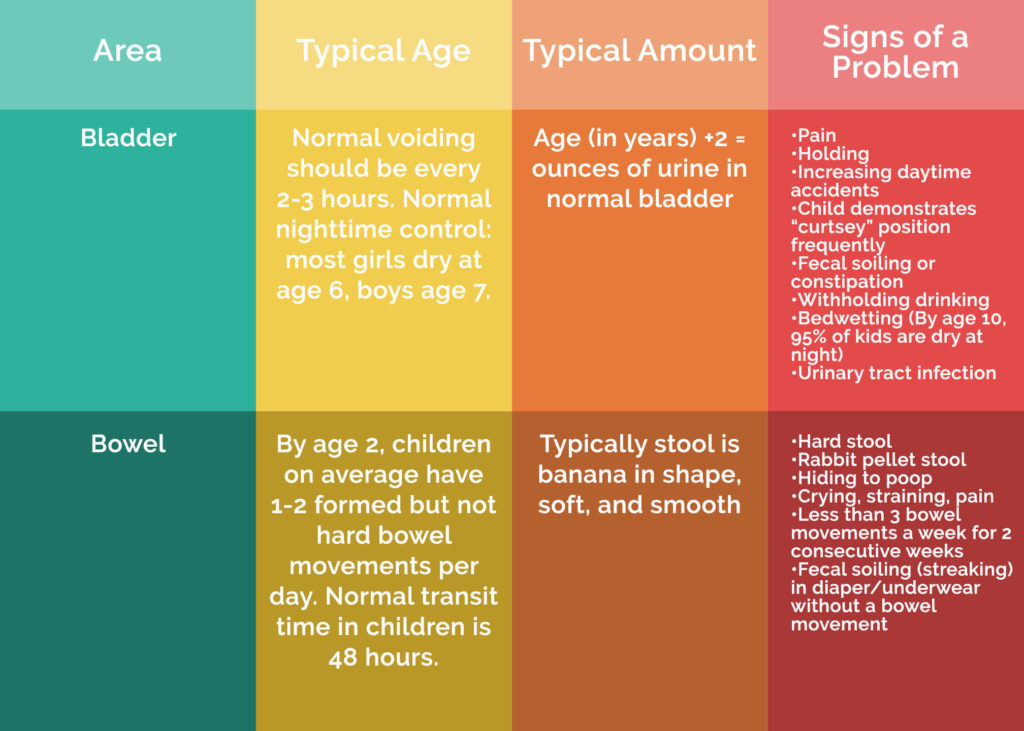
 Childhood bladder and bowel issues are more common than one would think. Understanding toileting accidents can help improve how you approach problems. I remember going through this experience with my own son and wondering what the heck was going on? He was 3 years old, and he would not poop. I knew he was scared. I knew he was getting stressed out. Also, I knew he was going up to 7 days without pooping!! I remember questioning if he needed more fiber, fluid, exercise. As time passed, I worried that there would never be a day when he did not need to take Miralax. I worried how much he was being mentally affected by all the stress around pooping. I think every family member weighed in at some time; all with good intentions but no real facts or practical help.
Childhood bladder and bowel issues are more common than one would think. Understanding toileting accidents can help improve how you approach problems. I remember going through this experience with my own son and wondering what the heck was going on? He was 3 years old, and he would not poop. I knew he was scared. I knew he was getting stressed out. Also, I knew he was going up to 7 days without pooping!! I remember questioning if he needed more fiber, fluid, exercise. As time passed, I worried that there would never be a day when he did not need to take Miralax. I worried how much he was being mentally affected by all the stress around pooping. I think every family member weighed in at some time; all with good intentions but no real facts or practical help.